Miscarriage
A miscarriage, or spontaneous abortion, is the loss of a pregnancy before the 20th week, affecting approximately 10-20% of known pregnancies. It often occurs due to chromosomal abnormalities in the embryo, but other factors such as hormonal imbalances, uterine abnormalities, infections, and lifestyle factors can also contribute. While miscarriages can be emotionally and physically challenging, they are usually not indicative of future fertility issues. Support from healthcare providers and family can help individuals cope up with the emotional and physical phase.
On this page
1. Symptoms of Miscarriage
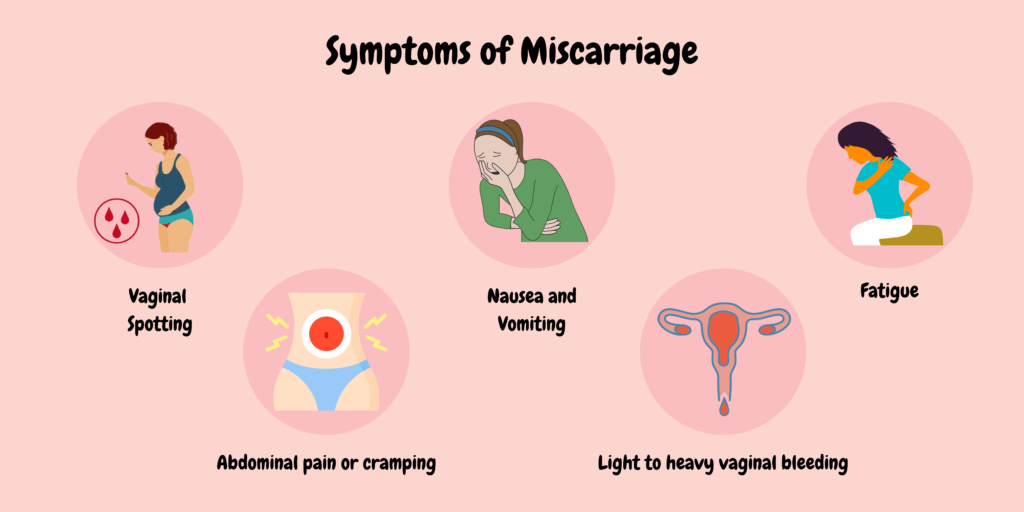
Symptoms of a miscarriage can vary, but common signs include:
- Vaginal Bleeding: This can range from light spotting to heavy bleeding.
- Cramping: Abdominal pain or cramping, similar to menstrual cramps, may occur.
- Tissue Passage: The expulsion of tissue or fluid from the vagina.
- Back Pain: Lower back pain can accompany other symptoms.
- Decreased Pregnancy Symptoms: A sudden loss of pregnancy symptoms, such as nausea or breast tenderness.
If any of these symptoms occur, especially in early pregnancy, it’s important to consult a healthcare provider.
2. Causes of Miscarriage

Miscarriages can occur due to a variety of factors, including:
- Chromosomal Abnormalities: Most miscarriages are caused by genetic issues in the embryo, preventing proper development.
- Hormonal Imbalances: Conditions like polycystic ovary syndrome (PCOS) or thyroid disorders can affect pregnancy.
- Uterine Abnormalities: Issues such as fibroids, septate uterus, or congenital abnormalities can interfere with implantation and growth.
- Infections: Certain infections, such as bacterial vaginosis or sexually transmitted infections, can increase the risk.
- Immune System Disorders: Conditions that affect the immune system may lead to pregnancy complications.
- Lifestyle Factors: Smoking, excessive alcohol consumption, drug use, and obesity can contribute to miscarriage risk.
- Chronic Health Conditions: Diseases like diabetes, hypertension, and autoimmune disorders can affect pregnancy viability.
- Advanced Maternal Age: Women over 35 have a higher risk of chromosomal abnormalities in embryos.
Understanding these causes can help individuals and healthcare providers manage risks and provide appropriate care.
3. Diagnosis of Miscarriage
The diagnosis of a miscarriage typically involves several steps:
- Medical History: The healthcare provider will review the patient’s medical history, including any previous miscarriages and current symptoms.
- Physical Examination: A pelvic exam may be performed to check for signs of miscarriage, such as cervical changes or tissue passage.
- Ultrasound: A transvaginal or abdominal ultrasound is often used to visualize the uterus and confirm the presence or absence of a developing embryo, assessing for signs of a miscarriage.
- Blood Tests: Hormone levels, particularly human chorionic gonadotropin (HCG), may be measured to determine if they are rising appropriately, which can indicate a healthy pregnancy or suggest a miscarriage.
- Follow-up Care: If a miscarriage is suspected, follow-up ultrasounds or blood tests may be conducted to monitor the situation and confirm the diagnosis.
These methods help healthcare providers ensure accurate diagnosis.
4. What happens to your body after a miscarriage?
After a miscarriage, a person’s body goes through several changes affecting the individual’s health. Here are some common aspects:
- Physical Recovery: The body may experience cramping, bleeding, and passing of tissue. These symptoms typically go within a few days to a couple of weeks, depending on how far along the pregnancy was.
- Hormonal Changes: Hormone levels, particularly human chorionic gonadotropin (HCG), will gradually decrease. This process can take several weeks, and some individuals may experience symptoms associated with hormonal fluctuations, like mood swings.
- Emotional Impact: Many people experience a range of emotions, including sadness, grief, anger, or guilt. You can take help from your support system or your partner for emotional wellbeing.
- Fertility Considerations: Most individuals can conceive again soon after a miscarriage, often within one to three menstrual cycles, but it’s advisable to consult a healthcare provider.
- Monitoring Health: Follow-up appointments may be recommended to ensure the body is healing properly and to discuss any ongoing symptoms or concerns.
5. Complications
Miscarriage can lead to several complications, both physical and emotional. Some complications include:
- Infection: Retained tissue after a miscarriage can lead to infections, which may require medical treatment, including antibiotics or, in some cases, surgical intervention.
- Heavy Bleeding: While some bleeding is common, excessive or prolonged bleeding may require medical attention.
- Emotional Impact: Many individuals experience grief, anxiety, or depression following a miscarriage.
- Future Pregnancy Risks: Although most individuals can conceive again without issues, some may experience recurrent miscarriages or other complications in subsequent pregnancies.
- Physical Health Concerns: In rare cases, complications such as uterine scarring may occur, potentially impacting future fertility.
- Psychological Issues: Some may develop post-traumatic stress disorder (PTSD) or other psychological conditions related to the loss.
It’s important for individuals who experience a miscarriage to seek support and follow up with healthcare providers to address any complications or concerns.
6. Prevention
While not all miscarriages can be prevented, there are several steps that individuals can take to reduce the risk:
- Healthy Lifestyle: Maintaining a balanced diet, exercise regularly, and achieving a healthy weight can promote overall well-being and support a healthy pregnancy.
- Avoiding Harmful Substances: Refraining from smoking, excessive alcohol consumption, and drug use is crucial. Limiting caffeine intake may also be beneficial.
- Managing Chronic Conditions: Proper management of chronic health issues, such as diabetes, hypertension, and thyroid disorders, can help reduce risks.
- Prenatal Care: Regular check-ups and prenatal care are essential for monitoring health and addressing any issues early.
- Genetic Counseling: For those with a history of recurrent miscarriages or known genetic issues, consulting a healthcare provider may provide insights and support.
- Stress Management: Practicing stress-reduction techniques, such as mindfulness, yoga, or counseling, can help support emotional health.
- Medication Management: Discussing all medications with a healthcare provider to ensure they are safe during pregnancy is important.
- Vaccinations and Infections: Staying up to date with vaccinations and avoiding infections can help protect pregnancy health.
Consulting with a healthcare provider for personalized advice and monitoring can also help manage risks effectively.