Ways of Delivery
Pregnancy is an exciting journey with ups and downs. A women go through many emotional and physical changes. There are several types of birth methods to choose from, which can be according to a women choice or the need for her body and baby. You should discuss the delivery methods with your healthcare provider for easy and smooth delivery.
On this page
What are the types of delivery in pregnancy?
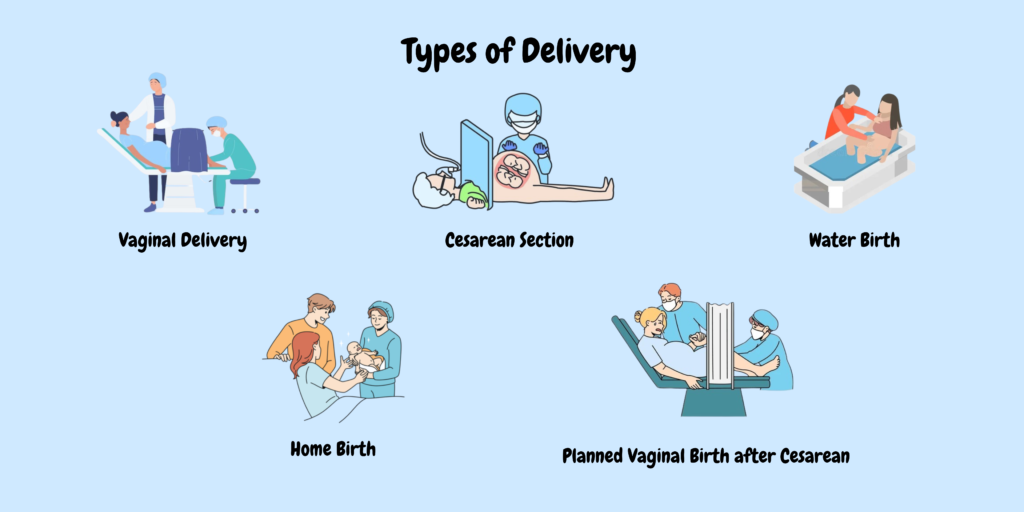
There are several types of delivery methods in pregnancy, stated as follows:
- Vaginal Delivery (Spontaneous Vaginal Delivery, Assisted Vaginal Delivery).
- Cesarean Section (C-section).
- Water Birth.
- Planned Vaginal Birth after Cesarean (VBAC).
1. Vaginal Delivery
It is the most common and natural method of childbirth, where the baby is born through the birth canal. Vaginal delivery can be spontaneous or assisted.
Spontaneous Vaginal Delivery (SVD):
Refers to the natural process of childbirth without medical intervention or assistance in starting the labor. This type of delivery begins when the body goes into labor on its own, typically marked by the onset of regular contractions and the gradual dilation of the cervix. Labor starts spontaneously, often indicated by contractions, the rupture of membranes (water breaking), or other signs such as nesting behavior or loss of the mucus plug.
Benefits:
- Shorter recovery time compared to surgical deliveries.
- Lower risk of infection and complications associated with surgery.
- Enhanced bonding opportunities immediately after birth due to skin-to-skin contact.
Risks: Although it’s safer, spontaneous vaginal delivery can involve risks such as perineal tearing, prolonged labor, or fetal distress.
Assisted Vaginal Delivery:
It is a type of childbirth in which medical tools are used to help the baby out of the birth canal during vaginal delivery. This method is typically used when labor is prolonged, the mother is unable to push effectively, or there are signs of fetal distress. There are several tools and procedures used to aid the baby out. They may include:
- Forceps Delivery: Forceps are spoon-shaped instruments that are gently placed around the baby’s head to help guide it out during contractions. This method requires the mother’s cervix to be fully dilated.
- Vacuum Extraction: A soft cup attached to a vacuum pump is placed on the baby’s head. Gentle suction is applied to help pull the baby through the birth canal during contractions.
- Episiotomy: It is a surgical procedure that involves making an incision in the perineum (the area between the vaginal opening and the anus) during childbirth. This procedure is performed to facilitate delivery and prevent tearing of the vaginal tissues, especially in cases where the baby is larger or in specific positions.
- Amniotomy: It is also known as artificial rupture of membranes, is a medical procedure in which a healthcare provider intentionally breaks the amniotic sac surrounding the fetus during labor. This is done using a sterile instrument, often referred to as an amnihook.
- Induced Labor: It refers to the process of artificially stimulating contractions in the uterus to initiate childbirth before natural labor begins. This may be necessary for various medical reasons, ensuring the safety of the mother or baby.
Benefits:
- Can shorten the duration of labor and reduce the need for a cesarean section.
- May help in cases of fetal distress, allowing for quicker delivery.
Risks:- Potential for injury to the mother, such as tearing or pelvic floor issues.
- Risk of injury to the baby, including bruising or, in rare cases, more severe trauma.
- Increased likelihood of a longer recovery period compared to a spontaneous vaginal delivery.
2. Cesarean Section (C-section)

A C-section is a surgical procedure used to deliver a baby through incisions made in the mother’s abdomen and uterus. This method is employed when vaginal delivery poses risks to the mother or baby or when complications arise during labor. C-section is done for several medical reasons.
- Fetal distress or abnormal heart rate.
- Breech presentation (the baby is positioned feet-first).
- Multiple pregnancies (twins, triplets, etc.).
- Maternal health issues, such as severe hypertension or active infections.
- Previous C-sections or uterine surgery that makes vaginal delivery risky.
- Prolonged labor or failure to progress.
- Umbilical cord issues.
C-sections can be planned (elective) or unplanned (emergency), and the decision is made based on the health and safety of both the mother and the baby.
Benefits:
- Can be life-saving in emergencies for both mother and baby.
- Provides a controlled environment for delivery.
- May be necessary for certain high-risk pregnancies.
Risks:
- Surgical complications, such as infection, bleeding, or injury to surrounding organs.
- Longer recovery time compared to vaginal delivery.
- Potential for complications in future pregnancies, including increased risk of placental issues or uterine rupture.
3. Water Birth
Water Birth is a method of childbirth that involves laboring and delivering the baby in a tub or pool of warm water. This approach is often chosen, because it provides a more soothing and comfortable environment for both the mother and baby. Many women choose to labor in water to help relieve pain and promote relaxation. The buoyancy of the water can reduce pressure on the body and may lead to a more manageable labor experience.
Benefits:
- The warm water can help alleviate labor pain and reduce the need for pain medication.
- Immersion in water can promote relaxation and a sense of calm.
- Water allows for greater freedom of movement, enabling mothers to find comfortable positions during labor.
- For some, water birth is seen as a gentler transition for the baby from the womb to the outside world.
Risks:
- Potential for infection if proper hygiene and protocols are not followed.
- In rare cases, complications may arise that require a necessary transfer to a hospital setting.
- Some healthcare providers may have concerns about fetal monitoring and the baby’s immediate response after birth.
4. Home Birth
A home birth is the refers to giving birth at home instead of a hospital or birthing center. Many women choose home birth to have a more comfortable, familiar environment with less medical treatment, but it is important to carefully consider the risks and benefits before making this decision.
Benefits:
- Many women feel more relaxed and are in control in their own home. They can move freely, choose their preferred laboring positions.
- Home births are typically attended by midwives who provide continuous, personalized care throughout labor and delivery.
- Home birth may reduce the likelihood of interventions like epidurals, C-sections, and inductions.
- Home birth can allow for a more family-focused experience, with the possibility of having loved ones present.
Risks:
- While most pregnancies progress normally, complications can arise unexpectedly, such as fetal distress, excessive bleeding, or problems with the placenta. In these cases, a quick transfer to a hospital is necessary. However, if the birth occurs too rapidly, getting to a hospital may not always be possible.
- At home, pain relief options like an epidural are not available.
- In a hospital, there are advanced medical tools and specialists available in case of complications. At home, these options may not be easily available.
- Home birth is generally not recommended for women with high-risk pregnancies.
5. Planned Vaginal Birth after Cesarean (VBAC)
It refers to the attempt to have a vaginal delivery after one or more previous cesarean sections. VBAC can be a safe option for many women, but it requires careful consideration and planning. Women with a single previous low-transverse C-section are often good candidates for VBAC.
Benefits:
- Vaginal births typically involve less recovery time and fewer complications compared to C-sections.
- Avoiding major surgery reduces the risk of infection, blood loss, and other surgical-related issues.
Risks:
- The most significant risk associated with VBAC is the possibility of the uterus tearing along the previous C-section scar, which can be life-threatening for both mother and baby. However, this risk is relatively low.
- If complications arise during labor, there may be a need for an unplanned C-section, which carries its own risks.
Going for VBAC is a safe choice for many women, but you should consult with your healthcare provider.